Prospective students who would like to enjoy a rewarding, fulfilling, invigorating healthcare career as a certified nursing assistant (CNA) in the Dallas / Fort Worth area of Texas now have a fast-track option that enables them to accomplish their occupational goals drastically sooner than average. The members of staff at Legacy Healthcare Careers Nursing Assistant School are extremely excited to introduce the 7-day CNA program.
The caring, professional instructors at Legacy Healthcare Careers Nursing Assistant School can assist prospective pupils to convert their career-oriented dreams into reality in as little as 7 days! Those who are ready and willing to devote one long week to their schooling can enter a new and exciting career pathway in only 7 days. Continue reading for more details about this innovative nurse aide training program.
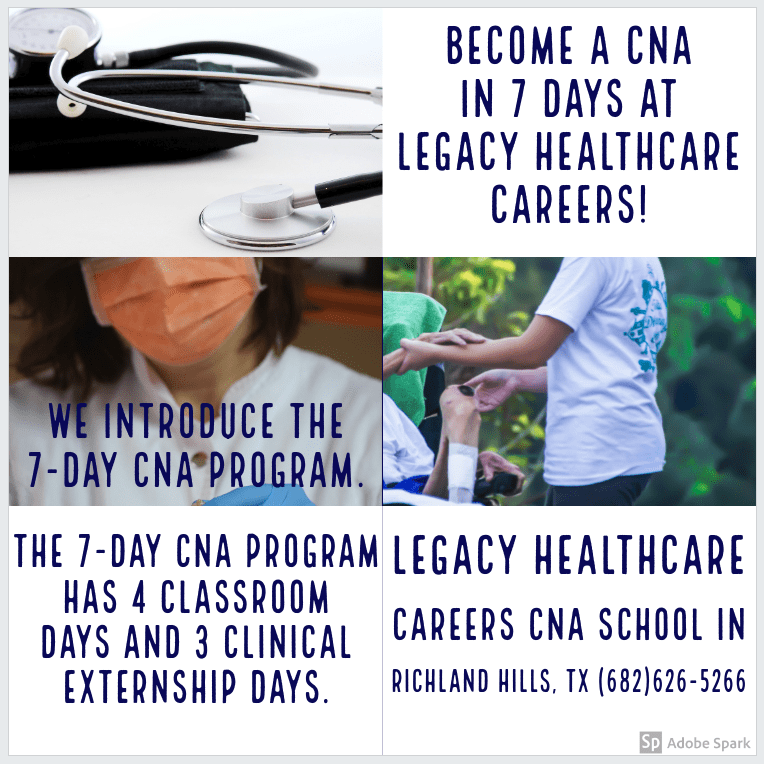
The 7-day CNA program entails attending school for seven long days in a row. The 7-day CNA program consists of four days of nursing assistant theory instruction in the classroom setting. The four days of classroom and lab instruction will be followed by three days of hands-on clinical practicum externship at a local healthcare facility in the Dallas / Fort Worth Metroplex area.
After successful completion of the one week of nurse aide training at Legacy Healthcare Careers Nursing Assistant School, students are considered official graduates who are now legally allowed to secure employment as nursing assistants. Once the nurse aide graduate takes and passes both sections of the CNA state test, he or she is granted state certification as a certified nursing assistant (CNA).
The CNA certification opens the doors to an amazing abundance of healthcare employment opportunities associated with steady income and job security. CNAs are in demand in most employment markets in Texas with employment numbers expected to be on the rise through the year 2026 according to projections from the United States Bureau of Labor Statistics.
In addition, due to longstanding reciprocity and endorsement agreements between nursing assistant registries and boards of nursing in different states in the US, the CNA certification bestows an array of marketable job skills upon the nurse aide graduate that can potentially be transferred from region to region.
Please watch the video below for more information regarding the 7-day CNA program. Moreover, interested prospective applicants should feel free to place a telephone call to Legacy Healthcare Careers Nursing Assistant School at (682)626-5266 to schedule a tour of the school and to inquire about enrollment. Prospective students should also feel free to submit an application to the CNA program online by visiting the school’s website at www.LegacyHealthcareCareers.com.